The Vicious Cycle of Itching and Scratching in Atopic Dermatitis
Previously, we discussed the two basic principles for controlling atopic dermatitis: “eating” and “scratching”. This article will explain why atopic dermatitis causes itching, and how to improve the “scratching itch” problem. For the “eating” part, you can refer to the article “Dietary Control for Babies with Atopic Dermatitis! Teach You How to Improve Your Baby’s Atopic Dermatitis Through Diet”.
The Patient’s Uncontrollable Scratching Behavior
For older children suffering from atopic dermatitis, the most unbearable symptom is undoubtedly the maddening itch. Even after taking strong corticosteroids to control skin symptoms, just one night of incessant scratching can quickly cause the skin lesions to flare up again. Therefore, how to resist the urge to scratch and have a good night’s sleep without scratching is the most important principle in controlling atopic dermatitis.
Scratching Wounds Lead to New Allergic Reactions
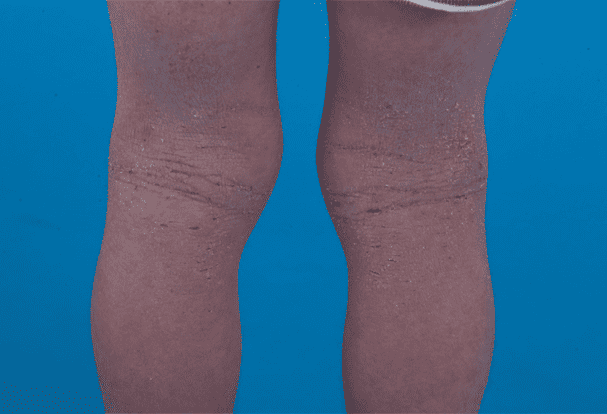
As the disease worsens, children will scratch more severely, resulting in numerous scratch marks and wounds on their bodies. In this situation, airborne allergens such as dust mites or bacteria on the skin like Staphylococcus aureus can enter the skin through these wounds, becoming new allergens in localized areas and causing inflammatory reactions and exacerbating the itching.
Among them, the role of Staphylococcus aureus in atopic dermatitis has gained attention in recent years. This bacterium secretes an “enterotoxin” that, upon entering the skin, causes significant inflammatory reactions, aggravating skin inflammation and itching. In severe cases, it can even lead to cellulitis, causing redness, swelling, heat, and pain that make the child extremely uncomfortable and, in severe cases, even sepsis, so it must be closely monitored and treated.
The Unique Nature of Staphylococcus aureus Enterotoxin
One might wonder why, among the many bacteria present on the skin, Staphylococcus aureus is particularly important. The main reason lies in the “enterotoxin” secreted by this bacterium, which possesses the unique property of being a “superantigen”.
Unlike regular antigens, superantigens do not require processing by antigen-presenting cells or binding to MHC Class II molecules; they can directly bind to T-cell receptors and stimulate a vigorous response and proliferation of T helper cells.
Conventional antigens must go through this processing and presentation process before being recognized and reacted to by T helper cells. However, superantigens can directly and efficiently activate large numbers of T cells, triggering a strong immune response, which is detrimental for atopic dermatitis patients who already have an imbalanced immune system.
Dust Mite Allergens Also Colonize Scratch Wounds
Of course, the wounds caused by scratching also allow airborne allergens like dust mites to enter the skin. In atopic dermatitis patients, where an environment of Type 2 helper T cells exists, the immune response to dust mites tends to develop in a pro-allergic direction, causing dust mites to become new allergens and triggering severe skin allergic reactions.
It is evident that, with multiple allergens simultaneously attacking, the child’s skin naturally becomes more red, swollen, and itchy, making it difficult to relieve symptoms and increasingly hard to control the urge to scratch, perpetuating this vicious cycle.
The Vicious Cycle Leads to Immune Imbalance
Once infected with Staphylococcus aureus, its enterotoxin enters the skin and becomes a new allergen, causing severe allergic reactions. The patient’s symptoms then worsen further, and the intense urge to scratch makes them unable to resist scratching, creating new wounds that allow more allergens and bacteria to enter the body, continuing the vicious cycle.
Research from National Taiwan University has found that in atopic dermatitis patients, Type 2 helper T cells are less likely to undergo cell death (apoptosis) when stimulated by Staphylococcus aureus enterotoxin. In contrast, the excessive Type 1 helper T cells in healthy individuals are more susceptible to enterotoxin-induced apoptosis. This suggests that Staphylococcus aureus enterotoxin exacerbates the imbalance between Type 1 and Type 2 helper T cells in atopic dermatitis patients, causing their allergic immune response to become even more dysregulated.
Emergency Control Measures
For atopic dermatitis patients covered in scratch marks and wounds with severe infections, clinicians’ emergency response is to bandage the more severe areas, combined with the use of topical and systemic antibiotics, to control the condition within a shorter time and prevent bacterial infections and allergen invasions from exacerbating flare-ups.
Sometimes, to prevent patients from unconsciously scratching their skin during sleep and worsening the rash, doctors may also recommend bandaging the more severe areas and having the child wear gloves to sleep while keeping their nails trimmed to prevent wounds from worsening due to scratching. Constantly emphasizing these daily details is more important than simply using medication, so we repeatedly remind parents to pay close attention to this aspect.
The Benefits of Dust Mite Control in Managing the Condition
Once wounds appear on the affected areas, not only can bacteria easily invade, but environmental dust mite allergens can also take advantage of the wounds to enter the body, becoming another source of allergens. Therefore, at this stage, if more attention is paid to controlling the amount of dust mites in the home, it can reduce the chances of dust mites entering the wounds, which can still be helpful in controlling the symptoms of atopic dermatitis.
Currently, there are many so-called anti-dust mite products on the market, such as anti-dust mite mattress covers and pillow cases. Although they cannot completely cure the condition, they can reduce symptoms by about 50%. However, it should be noted that using these products does not mean that the symptoms will disappear completely; they still need to be combined with other treatment methods to truly control this stubborn condition.
Why Air Allergens Cannot Improve with Age?
Many people wonder why food allergen-induced atopic dermatitis improves as the child grows older, but symptoms caused by airborne allergens like dust mites or bacterial toxins do not improve with age.
The main reason lies in the “oral tolerance” mechanism mentioned earlier. When children continue to consume relatively high doses of the same food allergen, their maturing immune system gradually develops tolerance to that food, causing symptoms to improve over the years.
However, for airborne allergens and bacterial toxins, children do not ingest large amounts of them orally during their growth and development, so they cannot develop the same oral tolerance, leading to persistent and recurrent flare-ups without the improvement seen with food allergies.
How to Prevent Children from Scratching Wounds?
Most children tend to scratch uncontrollably when itchy during sleep, which can easily lead to severe wounds. If necessary, consider giving them first-generation antihistamines that can aid sleep, taking advantage of their sedative side effects to improve sleep quality and reduce the chances of scratching.
Additionally, keeping children’s nails trimmed flat or having them wear gloves to sleep are effective ways to prevent severe scratching wounds. Parents should always be mindful of their children’s habits to avoid worsening scratch wounds.
If you want to know more, or want to browse more pictures, please click the video below: